
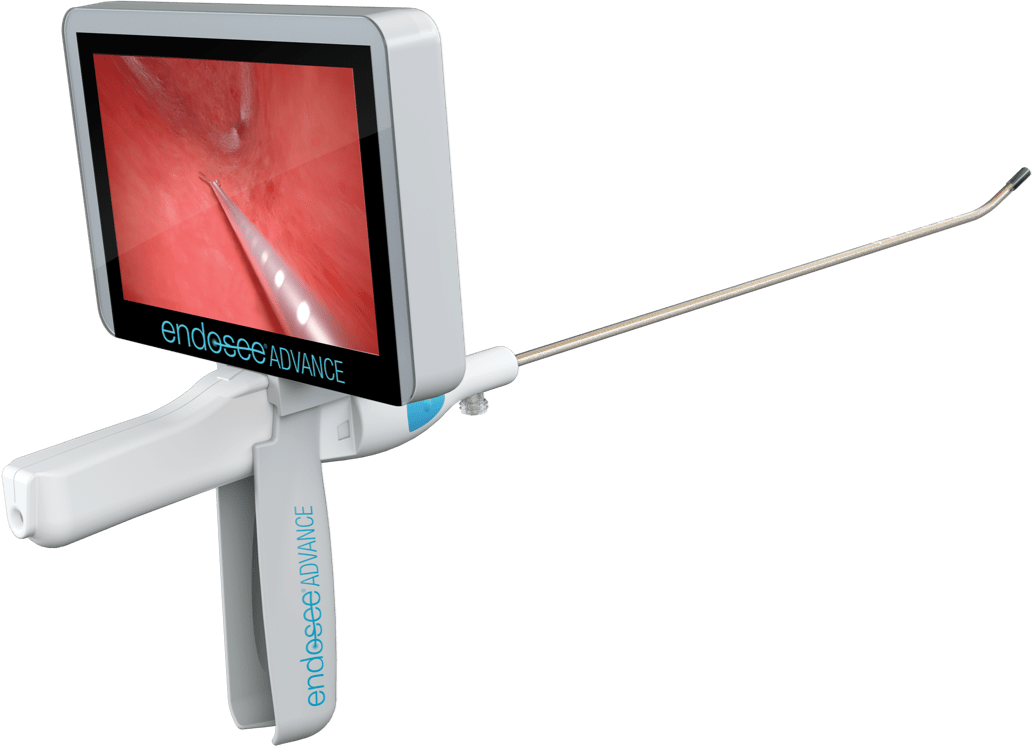
Endosee® Advance: A Low-Cost Advancement for Reimbursed Procedures
Direct endometrial evaluation with Endosee® Advance can help you provide a better standard of care at a better price to patients. Because procedures can happen in any exam room, Endosee® Advance can help patients avoid unnecessary OR intervention.


Avoiding OR intervention may save as much as $3,500 per patient1,2
Estimated calculation of savings in procedure charges of patients undergoing diagnostic office hysteroscopy who did not need to undergo OR hysteroscopy.
In a study of 130 patients at two outpatient clinics in academic university settings, 75 patients (57.7%) who underwent office hysteroscopy for abnormal bleeding did not need to undergo hysteroscopy in the OR. 55 (42.3%) patients underwent both inpatient and office hysteroscopy.
This represented an estimated savings of $1498 per patient (95% confidence interval, $1051–$1923) in procedure charges.
Among the 55 women who underwent OR hysteroscopy, there was 71% agreement between findings on hysteroscopy in the OR.
Reliable In-Office Use with a Reusable, Low-Cost Device
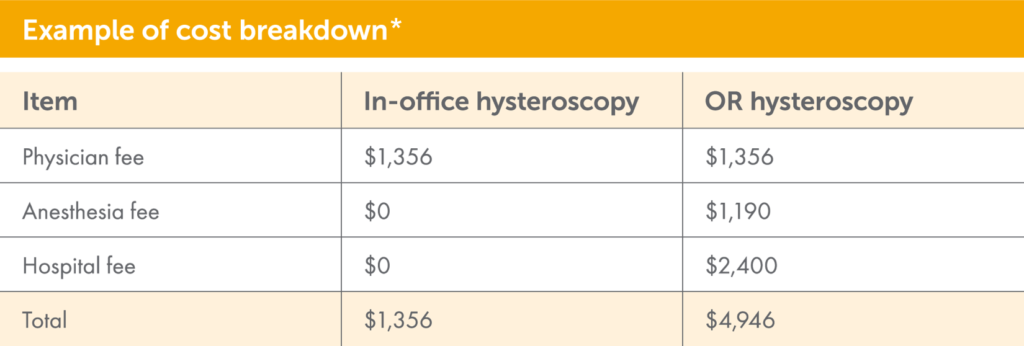
*The procedure cost for patients requiring both the in-office procedure and the OR procedure could be up to $6302.
Used in reimbursed procedures
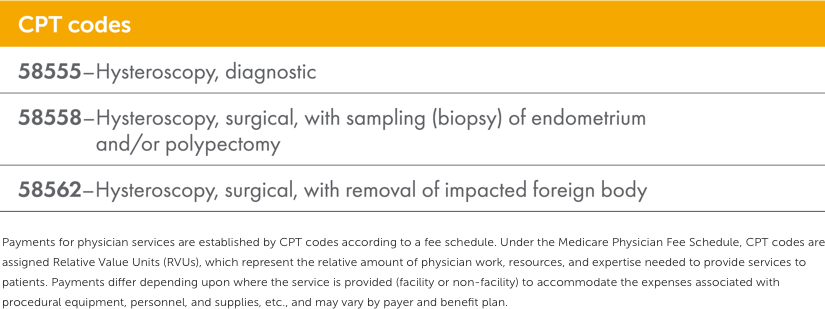

Helps you and your patients avoid the hassles and worry of delayed diagnosis 2,3
Immediate diagnostic information at the time of visit via Endosee® Advance helps reduce your patients’ worry and stress of waiting.2
Endosee® Advance can help reduce:
Extra appointments

OR costs

Wait times

Staffing allocation and training
Schedule conflicts
Sterilization costs

Explore Endosee® Advance

References
1. Goldstein SR, Anderson TL. Endometrial Evaluation: Are you still relying on a blind biopsy? OBG Mgmt Supp. 2017;10:S1-S4.
2. Moawad N, Santamaria E, Johnson M, Shuster J. Cost effectiveness of office hysteroscopy for abnormal bleeding. JSLS. 2014;18:1-5.
3. Isaacson K. Office Hysteroscopy: a valuable but under-utilized technique. Curr Opin Obstet Gynecol. 2002;14:381-385.
